The Future of Medicine | Tech Trends in Healthcare

As the future of medicine is tied to the growth of technology, it’s no surprise that AR and VR have become a big part of tech trends in healthcare. See the best cases of XR in medicine 👇
Although AR and VR are most commonly associated with entertainment, their potential reaches far more. Technology can become a significant factor in many places (like ecology) including the industry responsible for saving our lives. And with so many innovative projects, it seems that many already noticed the opportunities.
What does the future of medicine look like? We decided to ask those closest to the industry – people responsible for creating new tech trends in healthcare, and those who work with it day-to-day. Whether it’s taking care of patients’ mental health, working with AR during medical procedures or spreading awareness, all of them can significantly improve our health.
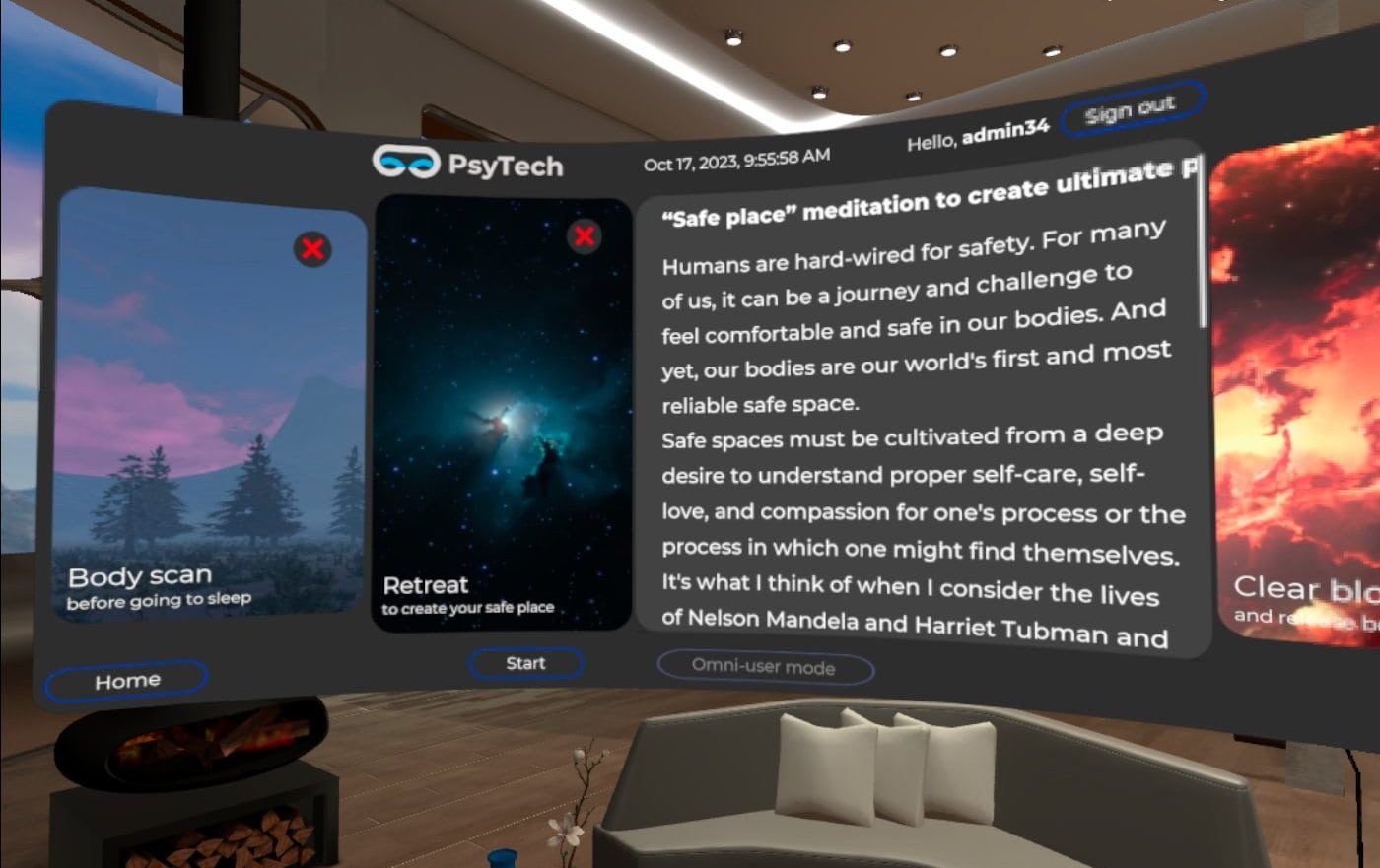
➡️ Daniel Andreev shared with us the story of PsyTech VR, a software supporting mental health through AR and VR.
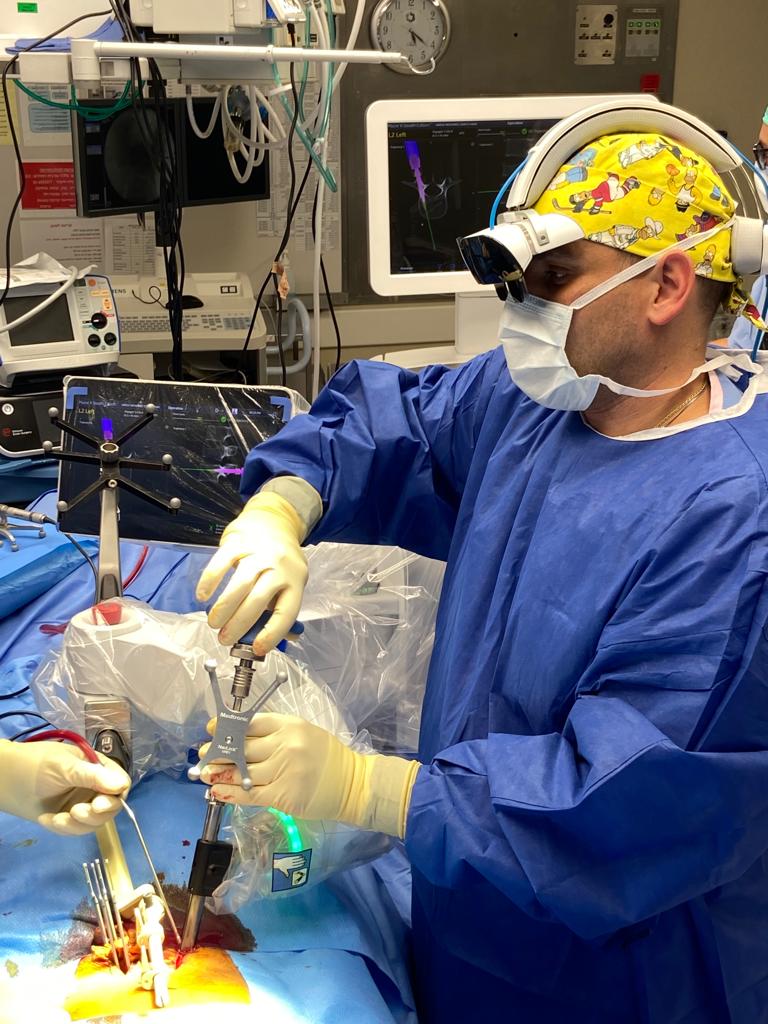
➡️ Dr. Cezar Jose Mizrahi told us about his own experience during cutting-edge AR spine surgery.
➡️ James Orrigo from Lad in a Battle unveiled the behind-the-scenes of AR effects created for the Brainstorm Summit, a gathering of professionals fighting pediatric cancer.
See how the future of medicine looks like 👇
PsyTech VR
 Daniel Andreev – Co-founder & CPO at PsyTech VR
Daniel Andreev – Co-founder & CPO at PsyTech VR
The Idea Behind the PsyTech VR and Possibilities For the Patients
The born of the use case
As an individual who has been involved in VR for four years, I have always been interested in the various use cases for this technology. While VR is widely used for gaming, real estate sales, and marketing, its applications in the healthcare industry are a relatively new area that emerged in the late 90s. VR is particularly helpful when it can solve a problem more effectively than traditional methods. There is evidence that it is a valuable tool for treating certain conditions.
PsyTech VR was inspired by a psychologist who recognized the potential of this technology. My mother, Inna, has been a cognitive behavioural therapy (CBT) counsellor and clinical psychologist for 16 years.
In 2020, while working at a clinic, she received a request to counsel a patient with acrophobia (fear of heights). The patient, who worked on a high floor of a skyscraper and was particularly afraid of panoramic windows with a bird’s-eye view of the city, contacted the clinic for help. Inna was assigned to counsel the patient, which was a routine consultation. According to the National Institute of Mental Health, around 12.5% of adults in the US experience specific phobias at some point in their lives, which means that consultations for phobias make up around 5-10% of consultations.
CBT counsellors typically use imaginal exposure therapy to help patients overcome specific phobias. This type of therapy involves the patient vividly imagining the feared object, situation, or activity. For example, a person with post-traumatic stress disorder might be asked to recall and describe their traumatic experience to reduce feelings of fear.
During the consultation, Inna used the imaginal exposure method, asking the patient to imagine standing on the roof of a skyscraper and looking down. However, not everyone has a vivid imagination, especially in an environment that traumatizes them. In addition, this therapy is time-consuming and can compromise the patient’s confidentiality. For instance, to overcome the fear of air travel, the therapist would need to accompany the patient on a flight, which is not always practical.
Unfortunately, the session ended earlier than expected. The patient was disappointed and left the office mid-session. The patient found it challenging to imagine the scenario and could not experience the real emotions as if they were looking at the view in person.
I was sitting at the dinner table with my father and our long-time friend, Peter Oykhman, waiting for Inna to come home. When she finally arrived, we could tell something was bothering her. Later, she confided in us about a negative experience she had gone through.
Inna suggested that it would be helpful if patients could teleport to a specific place where they could confront the object of their negative emotions in a safe way, similar to imaginal exposure but with a real-life component. We suggested the idea of using virtual reality instead, as it would provide the patient with a pre-made image rather than having to imagine it themselves.
I knew that we had the right idea – as at the right moment I was engaged in VR technologies being the Product Manager of the VR lab in the university for over the year. Thus was born an idea that soon became PsyTech VR. Peter, as the person who’s doing IT development for 30 years, immediately said that we’ll make the prototype within the next few months.
A few words about the history
Dr Aaron Beck coined Cognitive behavioural therapy (CBT) in the 1960s, and the first VR machine, Sensorama, was created by cinematographer Morton Heilig in the 1950s and patented in 1962. Sensorama was a large booth that could accommodate up to four people and combined various technologies to stimulate all of the senses. It featured full-colour 3D videos, audio, vibrations, smells, and atmospheric effects like wind.
Over the next 40 years, CBT gained widespread adoption and became the most popular approach approved by the WHO, while VR struggled to find its use case. However, in 1999, a group of psychiatrists and computer scientists from Emory University School of Medicine, Emory University School of Medicine, and Atlanta VAMC presented their work on Virtual Reality Exposure Therapy for PTSD Vietnam Veterans: A Case Study. The research showed that VR works for trauma therapy, and the study presented the results of the first Vietnam combat veteran with PTSD to have been treated with VRE. The patient was exposed to two virtual environments, a virtual Huey helicopter flying over a virtual Vietnam and a clearing surrounded by jungle. The patient experienced a 34% decrease in clinician-rated PTSD and a 45% decrease in self-rated PTSD.
Treatment gains were maintained at the 6-month follow-up. This groundbreaking study was a turning point for VR, as scientists and practitioners realized that it had the potential to be used in treating disorders. The basic idea is simple: if a person is afraid of something, such as spiders, they can put on VR glasses, find the creature in a virtual room, carefully examine it from all sides, or watch it descend from the ceiling on a thread of web. The patient’s task is to cope with their fear and take control of it. If they do everything correctly, the phobia will eventually disappear or at least become weaker.
According to scientists, VR therapy increases the effectiveness of treating anxiety disorders by up to 30% compared to traditional methods. It allows patients to transfer the internal processes of their psyche into an external, virtual environment, where they can work with their negative experiences outside of their heads.
After the Virtual Vietnam study, thousands of scientists began investigating the potential of virtual reality therapy. If you search for “VR therapy” on Google Scholar in 2023, you will find more than 300,000 articles published on the subject. The effectiveness of VR has shown the scientific community that PTSD is not the only use case, and other negative emotions, such as specific phobias, ADHD, autism, and schizophrenia, can benefit from VR therapy’s positive effects.

Find use case and use the momentum
PsyTech VR was founded after Inna, a CBT counsellor, encountered an issue that led to the discovery of a new opportunity. We realised that virtual reality (VR) can be used to promote peace and help people worldwide reduce anxiety and stress.
Our company was established in 2020, coinciding with the launch of Meta’s groundbreaking VR headset, the Meta Quest 2. We recognized the potential of standalone VR models like the Oculus Quest 1, which showed that the future of VR was standalone devices despite its CPU, battery, and tracking issues.
Despite the popularity of headsets that our competitors use – Pico g2 4K or VR cardboards using 3-Degree-Of-Freedom technologies, we chose to bet on the Meta Quest 2, which we believed was the most cutting-edge device available for the price. As it turns out, we were right. Within two years, Meta sold 20 million copies of the Meta Quest, making it the most widely sold VR device in history. During last Christmas, the Meta Quest was the most popular gift in the US.
Our VR platform, which features 6-Degree-Of-Freedom technology, allows users to navigate the virtual world using a full spectrum of movement. Users can use controllers to walk around, stationary boundaries to explore immersive environments, or even hand-tracking technology to interact with virtual objects, such as grabbing virtual spiders in our arachnophobia therapy. Our immersive technology allows users to observe MRI scans in virtual claustrophobia exposures or walk in a Japanese garden with blooming sakura in our travel therapy. All of this is made possible by the cutting-edge technology of Meta Quest 2.
PsyTech VR – the Swiss army knife of VR therapy
PsyTechVR is a leading XR company that specializes in developing VR/AR solutions for mental health and wellness. PsyTechVR offers scenario-based micro training using mixed reality (MX), combining virtual reality (VR). It targets anxiety, fear, phobia, PTSD, and OCD, delivering specialized therapeutic interventions through immersive simulations. PsyTechVR covers mental health and wellness immersive micro trainings are multi-level virtual scenarios mirroring real-life situations for anxiety, fear, phobia, PTSD, and OCD. They offer controlled exposure (CBT) and desensitization (EMDR) to triggers or stressors in a safe environment.
We are addressing the lack of accessible, engaging, effective mental health care by offering a virtual reality therapy system that provides personalised immersive experiences to help users overcome negative emotions, including fears, phobias, anxieties, anger issues, PTSD, OCD and practice mental wellness through relaxation techniques, breathing exercises and virtual travelling.
We’ve understood that The COVID-19 pandemic has emphasised the importance of accessible mental health care, with a rise in mental health disorders and 53% of US adults reporting negative impacts on their mental health due to pandemic-related stress. Our SaaS platform offers a personalised VR immersive multimodal perception experience tailored to each user’s needs and reduces barriers to non-pharmaceutical treatment for individuals who may otherwise face financial or geographical limitations.
Our XR platform is available to private practices of mental health practitioners, clinics, universities, and enterprises. It has the potential to revolutionise mental health and wellness care in the rapidly growing virtual reality therapy market.
When we compare PsyTech VR to a swiss army knife, we understand that our VR library is the largest available on the market and covers the following subjects:
➡️ The person can take a VR headset on the consultation with counselor, or during the self-guided trainnig from the comfort of home and experience the virtual triggers in a safe environment to overcome negative emotions – anxieties and stress.
➡️ In addition, PsyTech VR has developed an adaptive micro-training VR system that focuses on mental health and wellness. Our advisory team of psychologists found that during VR exposure therapy, users often face the challenge of the environment not aligning with their therapeutic needs and desires. To solve this, we made VR experiences adaptable to users’ needs with GenAI. PsyTech VR is the first company to integrate GenAI for therapy.
Recently, we have received the non-paid video review from James Husband – UK cbt/emdr counselor and the author of the Psychology on Demand YouTube channel. James explained how our AI can be used in the process of therapy.
Our SaaS platform offers an immersive multimodal perception experience in Virtual Reality that helps to remove barriers to non-pharmaceutical treatment for individuals who may otherwise face financial or geographical limitations. What’s available?
➡️ LMS platform with learning courses and questionnaires
➡️ 6-DOF VR application with CBT / EMDR protocols (40+ PTSD levels, 60+ fears and phobia levels, Five OCD levels, 15+ alcohol/cigarettes addiction, Five anger management levels, 1000+ relaxation places, mindfulness meditations, breathing relaxations, art therapy, body relaxation techniques)
➡️ Tool for onside, telehealth, and distant consultations/sessions
➡️ Dashboard with user statistics
➡️ The VR mask has integrated a biosensor for measuring HRV, pulse, stress levels, and concentration. Biosensors come with software.

The advantages of VR in the healthcare industry
Picture this: a world where the confines of traditional healthcare are transcended by the immersive embrace of Virtual Reality (VR). As I stand on the precipice of sharing insights into the realm of VR in healthcare, the tale unravels with promising numbers and transformative possibilities.
In the heart of the digital health landscape, where innovation dances with data, we find ourselves amidst a staggering growth trajectory. The ‘Global digital health market,’ a realm worth USD 262.63 billion in 2022, is set to unfurl its wings, soaring to an anticipated USD 939.54 billion by 2032. In the midst of this digital revolution, the U.S. digital health market stands as a testament, contributing a substantial USD 56.86 billion in 2022.
Now, let’s dive deeper into the enchanting narrative of Virtual Reality (VR) in healthcare. A realm once valued at USD 2.33 billion in 2022, VR in healthcare now spreading its wings, projected to grace the heavens with a valuation ranging from USD 3.11 billion to a breathtaking USD 25.22 billion by 2030. PsyTechVR, with its foresight, sees the stage set for a USD 7 billion spectacle in 2023, marking VR’s ascent to a pivotal role in healthcare.
But why the spotlight on VR in healthcare, you ask?
Step into the shoes of those seeking mental wellness, where PsyTechVR crafts tales of healing. VR, with its immersive charm, becomes a canvas for therapeutic interventions. Imagine confronting fears, unraveling anxieties, and battling phobias not in the dimly lit rooms of traditional therapy, but in the vivid landscapes of virtual reality. PsyTechVR’s ingenious use of VR, akin to a magical potion, addresses mental health with an unprecedented blend of personalization and adaptability.
This isn’t just about numbers climbing on a graph. It’s about breaking barriers, transcending borders, and making mental healthcare a tangible reality for everyone. As we emerge from the shadows of a pandemic-stricken world, the accessibility VR offers becomes a lifeline.
PsyTechVR’s SaaS platform, a beacon of hope, delivers tailored VR therapy experiences, democratizing mental health care.
But there’s more to this enchanting tale. Imagine a VR mask not just as a gateway to virtual realms but as a guardian, measuring heart rates, stress levels, and concentration. The integration of biosensors paints a new chapter, where data-driven insights guide both users and healthcare practitioners through the labyrinth of mental well-being.
As the ‘Global Virtual Reality (VR) in healthcare market’ continues its crescendo, we find ourselves at the dawn of a new era. VR, once a niche, is now the protagonist in the tale of healthcare transformation. With USD 7 billion on the horizon in 2023, the story of VR in healthcare is not just an expert opinion—it’s a saga of healing, accessibility, and the promise of a brighter, more immersive tomorrow.
AR spine surgery
 Dr. Cezar Jose Mizrahi, neurosurgeon
Dr. Cezar Jose Mizrahi, neurosurgeon
The Case of the AR-assisteed Back Surgery – Augmented Reality’s Role and Prognosis
Firstly, it is important to emphasize that AR has been used in minimally invasive spine surgery before, but according to Medtronic, the company that makes AR technology, this had never before been combined with robotic technology.
Without surgery, the patient had a high risk of further neurologic deficit, including paraplegia (unable to move his legs). The robotic arm achieves a three-dimensional recognition of the patient based on previously done scans. It achieves “perfect registration”, which gives the surgeon the ideal trajectory for their instruments. The AR technology further minimizes the risks of placing a screw on the spinal cord or nerve roots by allowing the surgeon to see the navigation system within the robot.
How does AR help with instrument positioning? Do you think it will increase the role of human surgeons or that it could supplement both human and robotic surgeries?
The experience of performing surgery equipped with an AR headset felt like being a combat pilot. I had all the patient’s vital information, including the CT images, displayed directly in front of me. I could look one way and see the lineup of the surgical screws that I had planned out before the procedure and then look down and see the surgical field magnified. The experience helped me perform the procedure exactly as I planned it, and only make adjustments that I might have felt necessary as the surgery developed. We’ve been seeing an increase in the use of robotic surgeries.
In my opinion, AR will be just another tool in the surgeon’s arsenal to achieve better results to our patients. I still do not see robotics, AR, or any other technology as a replace for the surgeon.
The AR device details – what information did it provide and how much training did it take to use?
You are able to see in real time: the coronal, sagittal and axial views. In addition, the AR headset worn on the surgeon’s head allows them to see all scans and pre-surgery planning that were uploaded before the surgery. You just move your eyes around this visual field — left, right, up and down — and you have everything. It’s like a PlayStation. As long it was the first time that robotics and AR were used in a real surgery, obviously, much of my training and adaptation were done in a lab.
I’m a neurosurgeon specialist in complex spine surgery and minimally invasive spine surgery since 2019. Regarding robotic spine surgery, I’m already familiar since 2017 but in the last few years, I decided to use it more and more. Today, it has become already a standard practice in my service. Regarding AR, it is still something new to me, and I just started to implement it in the last few weeks after a lot of research with the Mazor team.
Are AR assisted surgeries a recent phenomenon or have they been around for a while?
They already have been around for a while but as every new technology, we need to be very. careful implementing new practices. Safety first.
I am positive that AR and even VR will be soon a routinely tool in the medical practice. It includes not only surgeries but also trainees education, case evaluation and team discussion.
Brainstorm Summit
 James Orrigo, Social Entrepreneur & Motivational Entertainer from Lad in a Battle
James Orrigo, Social Entrepreneur & Motivational Entertainer from Lad in a Battle
What is the Brainstorm Summit?
The Brainstorm Summit is a gathering of individuals impacted by pediatric brain cancer, researchers, patients, families, scientists, and industry professionals in Washington, D.C., to wage the fight against childhood cancer.
I’m James Orrigo, and I had the privilege of kicking off the Brainstorm Summit with a truly unique showcase. We harnessed Augmented Reality to ignite new ideas, raise awareness and show how fun education can be by gamifying the medical field. I lead the Big Dreams Program, which empowers kids and teens affected by pediatric cancer to create their own animated videos, custom AR video games, and community-wide events that offer unforgettable support to patients and their families.
My journey has led me to work closely with families touched by pediatric brain cancer, particularly DIPG, a cancer that often robs young patients of their motor and cognitive abilities. Sadly, I’ve known too many of these incredible kids who have passed away. To make a difference, we must start with education and awareness. I visited a high school in New Hampshire and posed a challenge: How can we use AR to turn learning about DIPG into a game? The response was inspiring. Students brainstormed ways to utilize Snapchat filters to educate themselves and others about DIPG.
With the expertise of AR wizard Krunal Gediya, we crafted an experience that was not only educational and fun but also left you marveling at the possibilities right within your smartphone. At the Brainstorm Summit, I showcased this AR experience in style. Picture this: a giant brain, right in front of you, inviting you to step inside and use your hands to physically collect broken neurons and win educational cards.
AR played a significant role throughout the conference. We even collaborated with Aakash Mansukhani to set up a digital AR booth, accessible by scanning the back of a business card, where attendees could delve into the work we do with Children’s Cancer Research Fund. They could physically approach the digital billboards, meet the incredible children we support, and feel the call to get involved.

We also hosted nightly gaming sessions and workshops for patients who traveled to the summit. They played patient inspired AR games we had collaborated on with Eugene Soh, which are tailored to battling cancer and are limited mobility friendly. They could try on digital costumes, thanks to our collaborations with Jeetesh Singh and Krunal, and bring AR butterflies to life, courtesy of our teammate Krunal. Nights were filled with wonder and laughter, and the kids even had the chance to create their very own AR video game with the help of our teammate Florencia Raffa! The results were nothing short of incredible, igniting excitement about the boundless potential of AR. Attendees of the conference even had the opportunity to use an AR head tracking experience to promote their involvement at the summit thanks to our teammate Meet Kacha!
How can AR impact the healthcare industry?
The fusion of AR and healthcare is nothing short of fascinating. It serves as a positive distraction during treatments and procedures. It can educate patients about upcoming procedures or complex illnesses, all while turning learning into an immersive experience they’ll never forget. AR can also empower patients by giving them a sense of control. For instance, imagine punching virtual cancer cells, along with marshmallows and broccoli, with the force determining your score. This not only engages patients but also promotes mobility and blood circulation with limited mobility.
by ladinabattle
by Krunal MB Gediya
Moreover, AR can be a game-changer in the gaming realm. With head tracking, patients with limited mobility can steer their in-game characters simply by leaning their head or making facial expressions. This opens up a new world of gaming possibilities for kids who, due to their condition, may have thought they couldn’t play video games anymore.
In summary, AR holds incredible potential to revolutionize healthcare, offering solace, education, and even entertainment to those facing health challenges. It’s a realm of innovation where the possibilities are limited only by our imagination. It was such an honor to be able to bring this tech to this group and give a snippet of how we can use these tools for good.
VR and AR as the Future of Medicine
As impressive as they are, those are just a few of the examples of how technology can benefit the medical industry. Scientists and XR enthusiasts are taking it upon themselves to revolutionise healthcare, coming up with the most innovative designs. VR software for medical training, AR devices to track and visualise veins under the skin, or even gamified physical therapy can be commonly used by professionals even a few years from now.
While we see all of the projects from completely different angles, there’s one thing, we can all agree on: technology is rooted in the development of medicine. This leads us to the growing importance of AR and VR, making them inseparable parts of the healthcare industry. Its use – both practical and in marketing – can be a game changer when it comes to the future of medicine.
